With rural maternity wards closing, lawmakers hope funding will help
Listen
(Runtime 0:58)
Read
In the small town of Forks, Washington, on the Olympic Peninsula, expectant parents have no guarantee of a hospital birth. They have no guarantee of proper care for their newborn or for themselves. Instead, they have to drive hours away on winding rural roads to other hospitals or deliver in the emergency department.
Forks Community Hospital intermittently goes back and forth between offering labor and delivery care, and diverting patients to other hospitals miles away.
Right now, there is no date set for when the hospital will be able to open again for births, said Dr. Rebecca Pfaff, a family physician at the hospital trained in rural medicine and obstetrics.
Pregnant people nearing or in labor, or with potential other complications, come to the hospital and are treated as emergency room patients. Pfaff said the hospital will send these patients to a hospital with an open obstetrical department if they can.
The reason Forks Community Hospital doesn’t always offer these services is complex. One piece of it, Pfaff said, is financial. Medical reimbursement for obstetrical care is low.
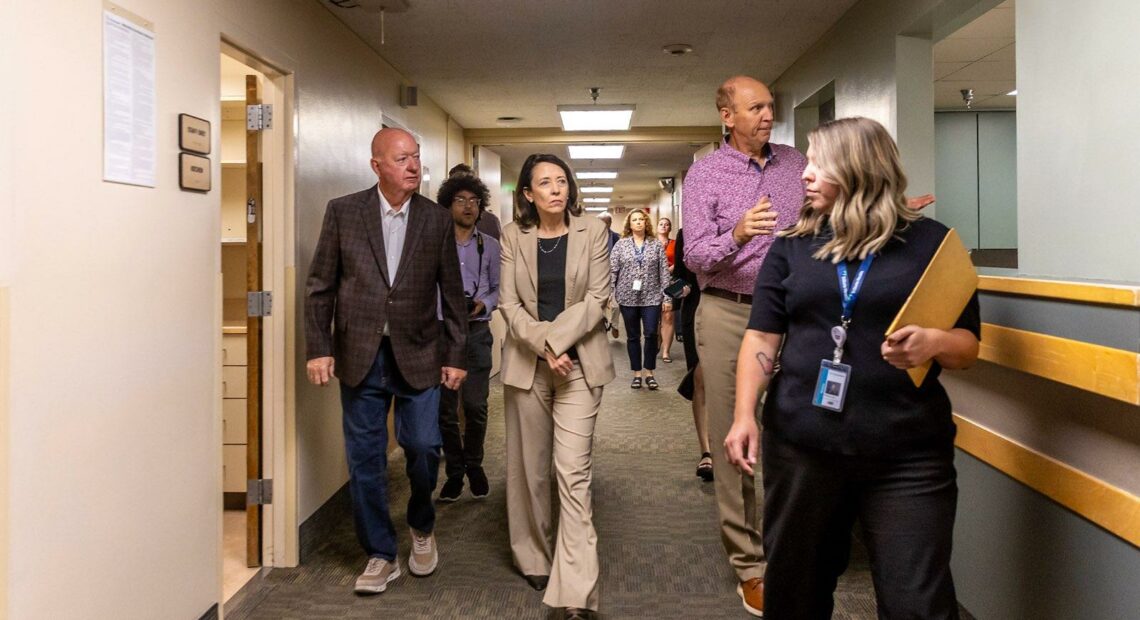
Sen. Maria Cantwell, of Washington, recently cosponsored a new piece of legislation that aims to increase rural hospitals’ reimbursements through Medicaid to help keep maternity wards open in rural communities.
“You have so many things that are challenging the delivery system,” she said. “The consequences are you have OB-GYNs leaving practices.”
Cantwell’s bill aims to stop that bleeding by giving rural hospitals and hospitals where a high percentage of births are Medicaid patients a 150% Medicaid reimbursement rate.
“You can have a population in some of our counties that are very big Medicaid, Medicare populations, and it makes the challenge of keeping a health care facility open harder,” Cantwell said in an interview with Northwest Public Broadcasting. “So, what we’re saying is, give them a little bit of a boost.”
Washington has seen a number of maternity wards close in recent years, such as Astria Toppenish Hospital’s in December 2022. Those in Forks and Bremerton are in a state of continuous diversion, meaning patients are transferred to other hospitals when possible.
Yet, providers said the money isn’t the only thing needed to keep these departments open and to provide the highest quality of care in small towns.
Staying ready, at a moment’s notice
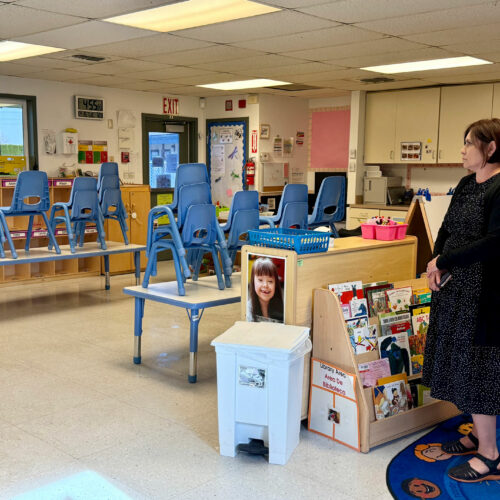
Port Townsend is east of Forks and in neighboring Jefferson County. Jefferson Healthcare is the only maternity ward within an hour for people living in the area.
The hospital doesn’t see a lot of births. Sometimes, it goes days or weeks without a delivery. This means physicians and nurses aren’t specialized to just obstetrics medicine. They practice medicine across the hospital, but still have to be poised to deliver at a moment’s notice.
The desire to practice a wide spectrum of medicine is what brought Dr. Joe Mattern to the hospital. A family physician, he delivered babies for about a decade before moving into administration. He is the hospital’s chief medical officer.
Providing obstetrics care in the community is essential to Mattern. He pointed to studies that show premature births go up in communities when maternity wards close. That often means more complicated prenatal care. Mattern also said that communities without labor and delivery units also have more emergency room births. That means less specialized staffing resources to deal with complications that can happen before, during and after labor for a mother and child.
The Cantwell legislation introduced earlier this month would help rural hospitals, which tend to have a lower share of private insurance payers, and make up for gaps in funding, Mattern said.
Small town hospitals have a cyclical problem: when they lack certain specialities, patients who can afford to will travel elsewhere for care. That means less money goes into the hospital, which makes it harder to train and retain specialized staff. The patients who can’t afford to go elsewhere are left behind. They might have more complicated medical conditions, due to a lack of access to care. Rural hospitals might not be able to meet their needs.
Funding would help. But, Mattern said there also needs to be a focus on training practitioners, especially those in rural settings, to be able to work in the full spectrum of medicine. He would like to see collaboration across the state to keep clinicians trained, and then have those trained staff in the right locations.
The bill would also allow obstetrics-trained providers from the U.S. Public Health Service to assist hospitals and states with “urgent maternal health care needs,” such as hospital closures.
The U.S. Public Health Service is a group of agencies within the Department of Health and Human Services focused on public health. Its work includes providing care in underserved communities.
When maternity wards close, Mattern said he fears physicians and nurses, who chose to practice in that field of medicine, will seek employment elsewhere.
“If suddenly they don’t have one part of their practice that’s really important to them, will they stay at that institution? Or will they go elsewhere?” Mattern wondered.
If they go elsewhere, the community loses out on access to other reproductive and prenatal care, and possibly primary care.
Going where you can do the work you love
With Forks diverting pregnant people to other hospitals, Pfaff weighs a lot of competing decisions. She loves where she lives.
“I get to drive through a national park, by a magical lake and through forests, to my little house,” Pfaff said.
She’s passionate about providing care there. Pfaff grew up just outside of the small town of Joyce, an hour from Forks in Clallam County. She chose to specialize in rural medicine, in part because she watched family members struggle to access quality health care where they lived.
“I have to choose between my chosen career path and my personal passions, and staying in the community that I want to be in,” Pfaff said.
If she stays in Forks and isn’t using those skills, she said she feels like she is denying another small community of this needed care.
Because ultimately, Pfaff loves labor and delivery.
“Delivering babies makes my heart sing,” Pfaff said. “I love delivering babies, it brings me great unabiding joy.”
Pfaff would like to see investment in continuous training for critical area nurses and physicians in this kind of medicine. That would mean sending these providers to work in central, higher volume areas to get real life practice when their hospitals aren’t doing as many births. A local coordinator could determine what hospitals need, so staff can feel confident when they do have to deliver.
The longer a hospital stays on diversion, the harder it is for staff to keep up the necessary skills for labor and delivery, Pfaff said.
Cantwell said she would support future initiatives to assist communities that have already lost their birthing centers. She noted programs that offer guidance and counseling for pregnant families as an example of something she would support.
Rachel Sun contributed to this report.