As the October 18 deadline approaches for state workers to be fully vaccinated, Washington’s Department of Veterans Affairs (WDVA) is putting in place contingency plans for staffing its four veterans homes.
The facilities, which are located in Port Orchard, Orting, Walla Walla and Spokane, serve about 400 veterans, spouses and widows of veterans and parents whose child died while serving in the military.
Recently, WDVA sent more than 150 separation letters to staff who’ve not yet confirmed they’re fully vaccinated. That’s about 16 percent of the agency’s workforce.
“Even though we have a concern with staffing, we’re still going to be able to run our normal operations come October 18th,” said David Puente, WDVA’s deputy director.
The contingency plan includes pausing all new admissions, relying on overtime, hiring contract staff and, as a last resort, temporarily transferring residents to community nursing homes, which face their own staffing challenges.
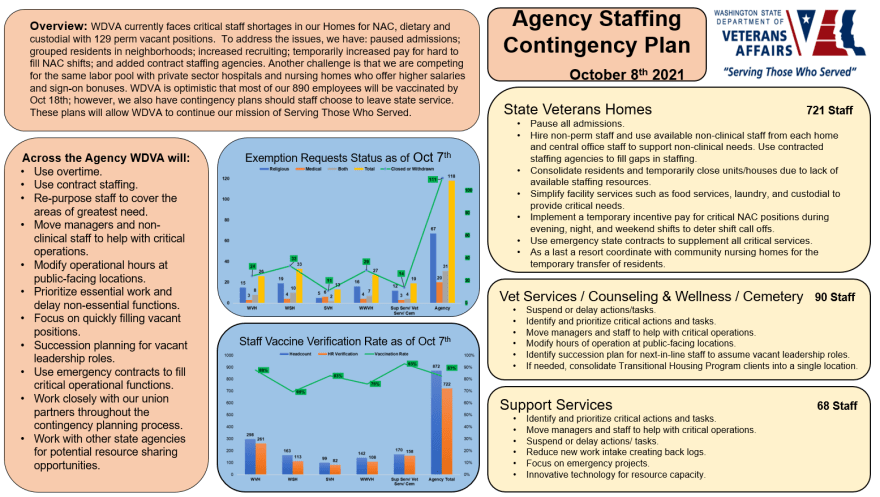
CREDIT: Washington State Dept. Of Veterans Affairs
Even before Gov. Jay Inslee imposed a vaccine mandate in August, WDVA was already struggling to recruit and retain staff. Recently, the agency said it was dealing with “critical staff shortages” at its veterans homes with 129 vacant positions.
If more employees leave due to the vaccine mandate, that will exacerbate the challenge. In the longer term, though, having all staff vaccinated could protect against future COVID-19 outbreaks in the homes.
The concept of state veterans homes dates to the post-Civil War era. In Washington, the first such home was the state’s soldiers home in Orting which was established in 1891 shortly after statehood. Oregon has two veterans homes that are operated by a third-party contractor.
As with many long-term care facilities, COVID-19 has hit state veterans homes hard.
Since the start of the pandemic, there’ve been nearly 200 positive tests among the roughly 400 residents in Washington’s four homes. Twenty-nine residents have died.
The most recent “fifth wave” of COVID-19, driven by the highly contagious delta variant, was less deadly because more than 90 percent of residents were vaccinated.
But many of the staff at the homes were slow to get the shots. As of August, the staff vaccination rate across the four homes was just 55 percent, according to WDVA data.
This summer COVID-19 once again got into the homes infecting both the vaccinated and unvaccinated.
From the end of July to the end of September, 41 of the nearly 200 residents at the Washington Veterans Home in Port Orchard and 15 staff tested positive for the virus. One veteran died.
It was a similar story at the Spokane Veterans Home where 34 residents and 23 staff have tested positive since July 21. Three veterans died.
Since July, Oregon’s veterans homes have reported 16 cases and no deaths, according to the Oregon Department of Veterans’ Affairs (ODVA). Since the start of the pandemic, there have been 13 COVID-related deaths at the Oregon facilities.
During the outbreaks in the Washington homes, most visitations were halted and residents were mostly confined to their rooms.
It was a frustrating time for Kris Boudreau, a 48-year-old Navy veteran who has multiple sclerosis, uses a wheelchair and lives at the Port Orchard home.
“A staff member will come in with COVID, they get tested and then they have it and then they go home and then we’re locked down for two weeks, completely shut down,” Boudreau explained.
He added that staff or visitors could have brought COVID-19 into the facility. Regardless, it meant Boudreau, who didn’t get sick, couldn’t see his daughter. They had to do video visits instead.
Puente, WDVA’s deputy director, agreed the last few months have been “challenging” at the homes.
“It was stressful,” Puente said. “For us, the common goal was to provide the residents with primary care and safety, as well as our employees, to ensure that we’re doing the best that we can possibly to honor our veterans and their families.”
Even with most of the residents vaccinated, the delta variant proved highly contagious.
“Once COVID is in the facility, it’s really hard to get it out of the facility,” said Cassie Prather, an epidemiologist at the Spokane Regional Health District.
In an interview, Prather described a “mad dash” to contain the outbreaks at the Spokane Veterans Home. Staff had to set up COVID-19 isolation units for those who tested positive and separate quarantine units for residents who were exposed. In addition, they had to once again wear full personal protection equipment, including respirators and gowns.
The chaos of the summer has passed. As of October 8, WDVA was reporting just two active COVID-19 cases among veterans home residents. The agency also said 83 percent of the staff is now fully vaccinated.
“We still have some work to do,” Puente said, referring to the percentage of staff who are vaccinated.
In Oregon, more than 90 percent workers at the state’s two veterans homes are either fully or partially vaccinated, or have received an approved exception, according to ODVA.
Oregon officials said they’re not expecting a significant loss of staff due to vaccine mandates.
In Kitsap County, where the Port Orchard veterans home is located, chief health officer Dr. Gib Morrow is also optimistic the requirement to get vaccinated won’t significantly deplete the healthcare workforce.
He said that while the mandate may “push some people out the door,” the bigger threat to staffing levels is COVID-19 itself.
“So many unvaccinated staff in healthcare have been sick and quarantined and are out,” Morrow said.
Still, resident Kris Boudreau is worried. He said he’s watched as staffing has gotten tighter and tighter since he first moved to the home in 2017.
Now Boudreau, who’s immunocompromised and recently got his COVID-19 vaccine booster shot, is bracing for more staff attrition after October 18.
“We’ve already lost some good people because they didn’t want to get vaccinated,” Boudreau said.