4 Ways Our Understanding Of The Coronavirus Has Changed A Year Into The Pandemic
BY ISABELLA ISAACS-THOMAS / PBS NewsHour
This month marks one year since the coronavirus pandemic swiftly upended daily life in the United States. In 2020, March brought about emergency declarations and indefinite school closures, followed by record unemployment claims and dozens of stay-at-home orders. By the end of the month, millions of people were either told to stay inside under lockdown or continue carrying out work deemed essential to keep society running.
At the time, terms like “social distancing” and “quarantine” were just beginning to shape our early pandemic lexicon, and masks had yet to become a staple of public life. Given the feelings of shock, loss and anxiety that so many have endured over these past 12 months, this dark anniversary may dredge up a complicated mix of emotions.
The reality is that more than 520,000 people have lost their lives to the coronavirus in just over a year, an immense toll that the nation will feel for decades. In the midst of that grief, it’s still worth noting how different this spring looks compared to the last. A tireless global scientific and medical research effort has paved the way for a present where millions are vaccinated every day. Those who do become ill also have a greater chance of surviving thanks to life-saving treatments.
ALSO SEE: Coronavirus News, Updates, Resources From NWPB
A year into this pandemic, we have the opportunity to reflect on the crucial breakthroughs that have shaped our response to the coronavirus, as well as how we’ve in some ways failed our most vulnerable. Here’s a look at what we’ve learned about this virus — how it spreads, what it does to the body and how we can outsmart it — and how the pandemic became the latest in a long line of historical events to highlight deeply-rooted racial and socioeconomic inequity in this country.
The coronavirus can be unpredictable, but we’ve learned how it spreads
Researchers have made remarkable progress in solving the many puzzles the coronavirus has presented, but some still remain unanswered.
We now know that the virus spread across the globe so efficiently in part because of its ability to be transmitted by asymptomatic or pre-symptomatic people — those who are infectious in days leading up to the onset of symptoms associated with COVID-19. Both groups may not be aware that they’re infectious, meaning they could be less likely to take precautions that prevent transmission.
It’s not yet entirely clear how much asymptomatic or pre-symptomatic spread contributes to case counts. But at least one recent study from the CDC suggests that asymptomatic carriers could account for more than half of all transmissions.
The reality of superspreaders, or the small fraction of COVID-positive people who account for a disproportionate number of new infections, presented yet another complication when it comes to controlling the coronavirus.
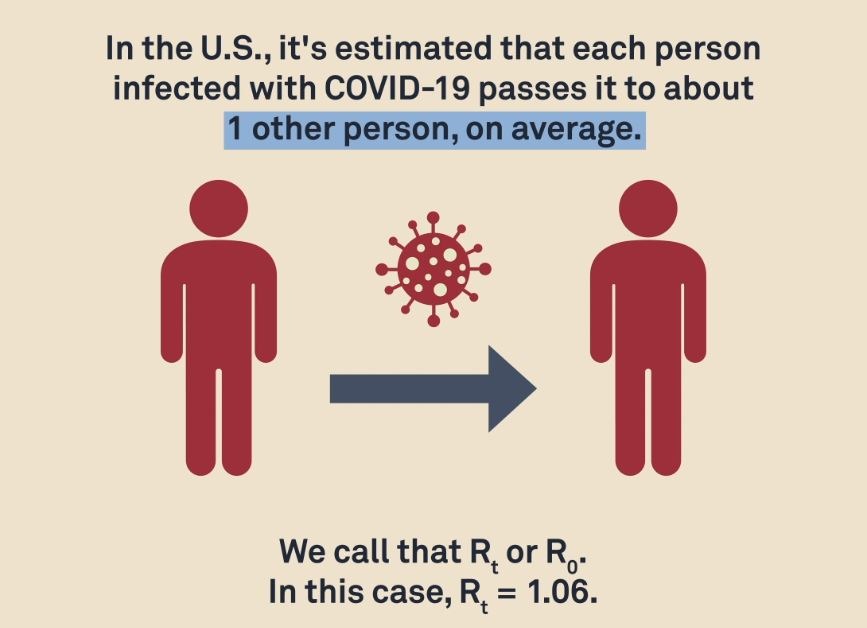
While it’s estimated that an infected person in the U.S. passes COVID-19 on to one other contact on average, some transmit the disease to far more people. Although there’s no strong consensus among scientists yet, research from Hong Kong last year estimated that just 19 percent of cases caused 80 percent of local transmissions, while around 70 percent of cases didn’t transmit the virus at all.
That phenomenon helps explain “superspreader events,” which researchers suspect happen when an infected person who is shedding a large amount of virus infects a disproportionate number of fellow attendees.
“If you’re just the unlucky one that’s in the room with one of those people at that time, and you breathe the same air, there’s a good chance you’re going to get infected,” said Kim Prather, an expert in atmospheric chemistry at the University of California San Diego.
In addition to confusing transmission patterns, the toll the coronavirus takes on those who become infected varies dramatically. Some COVID-19 patients get severely ill, and others don’t. A yet-unconfirmed portion of survivors, estimated now to be about 10 percent, experience lasting symptoms weeks and months after most people recover.
CREDIT: Megan McGrew/PBS Newshour
That condition is now known as PASC, or “post-acute sequelae of COVID-19.” Those who have it are more commonly referred to as “long haulers.” Patients with PASC range in age and health status — some people with generally moderate disease and no pre-existing conditions come down with it, while others have been hospitalized or even intubated during the first few weeks of their illness.
The symptoms endured by these patients range from persistent fatigue, memory loss or “brain fog,” and anxiety to shortness of breath, headaches, muscle and joint pain, among other seemingly disparate manifestations of the illness, according to Dr. Carlos del Rio, a professor of medicine at the Emory University School of Medicine.
“I think the number of people [with PASC] that will need care may be a lot bigger than we think it is,” del Rio said.
It’s still not clear how long those symptoms will last, or whether the condition may be permanent. The National Institutes of Health recently announced a new research initiative that will seek to answer why some patients contract “long COVID” while others don’t, and whether having COVID-19 itself increases one’s risk of other health conditions.
Doctors have learned how to better treat COVID-19 patients
When waves of severely ill COVID-19 patients began streaming into American hospitals last spring, health care workers didn’t yet understand why this new virus was making them so sick. Early data from other countries offered some perspective on factors like age and comorbidities, but there was no guidebook that doctors could use to treat the disease.
But robust global research efforts have since given physicians valuable insight as to what the coronavirus does to the body, and what providers can do to address those impacts.
ALSO SEE: Coronavirus News, Updates, Resources From NWPB
“Over the past year, we’ve gained a better understanding of seeing who is high risk for developing severe disease and how to optimize supportive care for those patients and then figuring out what treatments can help them recover sooner,” said Dr. Tomeka Suber, an assistant professor at the University of Pittsburgh School of Medicine.
Understanding how this disease impacts the immune system was a key revelation that allowed physicians to better treat COVID-19. “Cytokine storms” can occur when a severely ill patient’s immune response goes into “overdrive,” prompting “systemic inflammation” that can cause a lot of damage to the body, Suber said. In the case of the coronavirus — a pathogen their bodies had never encountered before — their immune systems are doing everything they can stop the coronavirus from replicating and infecting health cells inside their bodies.
“But the things that your immune system can make to fight the virus can also cause tissue injury, can cause lung inflammation, can cause kidney injury [and] can cause your blood pressure to get low,” Suber explained. “And if your [immune] response is not effective in controlling the virus, then ultimately the virus will continue to replicate and promote more inflammation and ultimately lead to severe disease, and sometimes death.”

Sisters Seri Sedlacek, left, and Susan Simpkins look in on their father, Chuck Sedlacek, at the Life Care Center, Wednesday, March 18, 2020, in Kirkland, Washington. CREDIT: Elaine Thompson/AP
Among the medicines that have emerged in the past year to treat COVID-19, steroids like demamethasone were the real “game changer” as far as reducing a hospitalized patient’s risk of being put on a ventilator or dying from the disease, Suber said. Those drugs can reduce the inflammation caused by a dangerously-heightened immune reaction.
Anticoagulants have also become a useful treatment for hospitalized COVID-19 patients who may experience clotting during the course of their disease, she said. Clotting can worsen dangerously low blood oxygen levels that are already associated with severe illness.
In addition to drugs that have been identified for critically ill patients, treatments designed for those who are still in the early days of their disease progression have been heavily researched over the past year. One such treatment, called monoclonal antibodies, works by recognizing the coronavirus’s infamous spike protein and blocking it from entering healthy cells, which can help improve a patient’s immune response.
Monoclonal antibodies are not widely available — the nation does not have enough to supply the treatment to everyone who could qualify for it. As variants of the virus continue to emerge, a persistent concern will be that one or more of those variants could evade existing treatments. One main goal for researchers moving forward, Suber said, will be to develop a variety of monoclonal antibodies that will be able to recognize and target different variants if that happens.
“That’s where the field is trying to move, because the virus is obviously adapting globally and we’re seeing these different variants develop,” Suber explained.
Suber expects to see more vaccines approved in the coming months, and hopes that they will be distributed widely so that a maximum portion of the global population is eventually protected against this disease, which also reduces the opportunity for new variants to crop up.
The effort to determine how best to treat COVID-19 is also far from over. Suber said researchers are continuing to work toward better therapies for patients that can reduce their chances of dying, becoming severely ill or even developing PASC.
“[It’s about] just being creative and developing these other therapies so that we can help patients recover from disease,” Suber said, adding that another key element of this approach will be to ensure that any safe and effective therapy developed for COVID-19 is “accessible to as many people as possible.”
Masks work to prevent transmission
Among the key facts we now know about the coronavirus, one significant truth stands out: masks work. In the months since public health officials like Dr. Anthony Fauci recommended wearing masks to slow the spread of the virus, the practice has become a prominent facet of public life in the U.S.
“What’s been clear to me is that you could go about your day to day business — wear a mask, maintain distance, decrease density in spaces — and the safety is quite good,” said Dr. Preeti Malani, chief health officer and a professor of medicine in the infectious diseases division at the University of Michigan.
That knowledge has allowed us to move away from surface-driven precautions like sanitizing groceries, a measure that many followed in the beginning of the pandemic, and start focusing on figuring out how to avoid breathing in other people’s air. Now, it’s common for businesses like supermarkets to feature social distancing markers that keep patrons six feet apart from each other, and masks are required to enter virtually any public space.
As more transmissible variants continue to spark concern over the possibility that they could contribute to yet another surge in cases, masks will remain a highly important tool to reduce the spread of the virus. The CDC recently recommended layering a surgical mask under a cloth one to maximize protection.
“The playbook to prevent transmission” of this virus hasn’t changed, Malani said, even in the face of variants. Although the “room for error” that comes with an ill-fitting mask or insufficient distancing may be smaller because many of these variants are more contagious compared to earlier ones in circulation, we still have the tools we need to keep our communities safe when we use them correctly.
Prather co-signed a letter to the Biden administration last month urging officials to address “inhalation exposure” and the important roles that high-quality masks, air filtration and ventilation play in preventing transmission. She argues that all three of those measures should be front and center in any reopening protocol. CDC guidelines for schools that are preparing to reopen lay out ways to prioritize ventilation, including by “opening windows, using portable air cleaners and improving building-wide filtration.”
There’s some dispute among the scientific community as to whether COVID-19 should be classified as an airborne illness — one that is primarily spread through smaller aerosols that can travel long distances as opposed to larger “droplets” that only make it a few feet before dropping to the ground — but experts agree that you’re far more likely to contract the virus from a nearby person rather than by touching a contaminated surface.
“What no one will argue with you on is that it’s inhalation. That is the primary way [transmission occurs,]” Prather said. “Then you can get in a fight about whether you should call it an aerosol or aerosol particle or a droplet.” Ultimately, she added, “you just want to protect against breathing [any viral particles] in.”
The virus exacerbates longstanding social and health disparities
The early days of lockdown prompted questions that many people didn’t have to consider day to day: What is the “essential” work that must continue when so much of the country has been shut down? What are the consequences when people in those industries — who did not sign up to keep American society functioning through a crisis — suddenly have to choose between their health and their livelihood?
The social divide between those who have the opportunity to work from home and those who don’t is particularly stark when the data is broken down by race and ethnicity. According to the CDC, people of color are “disproportionately represented in essential work settings.” The Economic Policy Institute reported in June that Black workers in particular are more likely to work frontline jobs in public transportation, the postal service, health care and other sectors.
The CDC also states that essential workers may face greater risk of being exposed to the coronavirus given the public-facing nature of their work, their inability to do their work from home and the fact that many of these employees don’t have access to paid sick days. But it’s not just occupation that’s made Black, Latino as well as Indigenous people in the United States more likely to contract, be hospitalized with or die as a result of COVID-19.
Dr. Utibe Essien, an assistant professor at the University of Pittsburgh School of Medicine, has for years studied social factors that are associated with health inequity — the same ones that have gotten a renewed spotlight during the pandemic.
When early data emerged from China suggesting that people with chronic illnesses like diabetes, obesity and hypertension were at a higher risk of suffering severe outcomes from the new virus, Essien and his colleagues were well aware of the fact that people of color were more likely to have those underlying medical conditions that put them at higher risk.
“We’ve seen the real horror that those preexisting conditions, those social determinants of health that have really come to the forefront [during the pandemic] have placed in marginalized communities due to COVID-19,” Essien said.
The systemic oppression that Black, Latino, Indigenous and other people of color in the U.S. face on a regular basis, the CDC notes, can “lead to chronic and toxic stress” that contributes to poor health. That oppression also shapes socioeconomic factors that put members of those communities at a higher risk for COVID.
ALSO SEE: Coronavirus News, Updates, Resources From NWPB
But this pandemic is only the most recent example of these truths coming into focus. During the 2009 H1N1 flu pandemic, Black and Latino people in this country were also more likely to contract that virus, be hospitalized or die from it. Essien said he was surprised to see that some people were shocked by the fact that Black and brown communities are suffering so greatly as a result of the coronavirus given that “decades and centuries of disparity” laid the groundwork both for this moment and the ones that came before it.
Moving forward, he hopes that the renewed attention on deeply-rooted health and socioeconomic inequities that jeopardize the health and wellbeing of people of color in America will be addressed even when this virus is behind us.
“We can’t just keep replaying the same lessons and have this element of surprise where we’re so shocked and awed at the disparities but actually go back to the literature, go back to the history and say, ‘Hey, we have the tools, we have what we need for this moment. Let’s learn from history rather than letting it repeat itself so painfully,’” Essien said.
Copyright 2021 PBS NewsHour. To see more, visit pbs.org/newshour