
COVID-19 Vaccinations Are Off To A Slow Start — But Not In Some Rural Areas
LISTEN
BY KIRK SIEGLER
In the small town of Oak Creek, Colo., — a three-hour drive from Denver, assuming the roads are clear — Gene Bracegirdle, a firefighter and EMT in training, is getting his first dose of the Moderna COVID-19 vaccine.
“The fact that it is here is kind of mind-blowing, like, they care enough to reach out to the rural communities,” Bracegirdle says.
The vaccine arrived in Oak Creek via a blue igloo cooler in a new mobile clinic set up by the local Routt County health department. Officials used CARES Act money to get things going. The task at hand is huge. Health officials must distribute the shots to a population of about 25,000 people spread across 2,300 square miles of northwest Colorado.
ALSO SEE: Coronavirus News, Updates, Resources From NWPB
“It’s exciting to see the initiative being taken,” Bracegirdle says, who is relieved to have gotten one this soon.
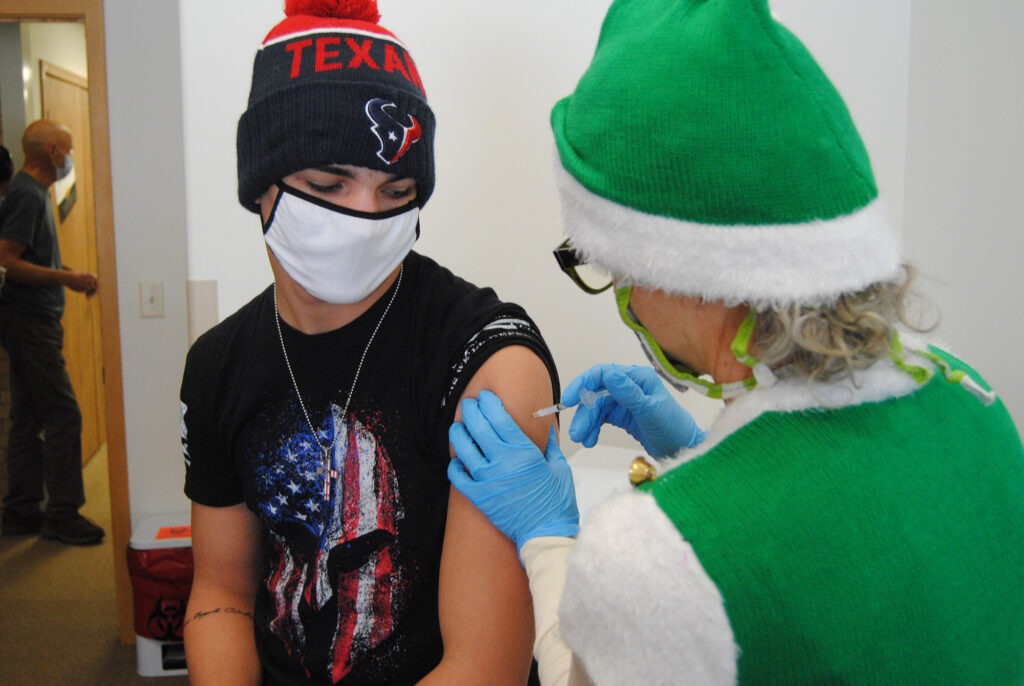
Gene Bracegirdle is relieved to get his first dose of the vaccine recently in rural Colorado.
CREDIT: Matt Bloom/KUNC
In many parts of the country, the rollout of COVID-19 vaccines has been sporadic, if at times, chaotic. But some rural communities, where health care has historically been harder to get, are reporting success stories in the initial phases.
“It’s early, but I think what we can take away from these past two weeks is states that place a priority on rural tend to have a successful rural rollout,” says Alan Morgan, CEO of the National Rural Health Association.
Morgan says some rural communities also just have fewer logistical hurdles to deal with and smaller numbers to get vaccinated.
That could be the case in Kittitas County, Wash. Public health officials there are reporting they’ve now offered the shots to almost all of their front-line essential workers, nursing home residents and staff. More than 1,300 people have taken it, with those numbers expected to grow further Friday.
“In terms of complexity and scope of the problem, we’re not dealing with something like a King County [in] the Seattle area,” says Rich Elliott, the county’s point person for vaccine distribution.
Elliott also happens to be the deputy fire chief in Kittitas, which has had a lot of recent wildfire emergencies. Emergency management officials were able to adopt quickly many of the same protocols and triaging from those wildland fire response plans and shift them to vaccine distribution.
They’re now in the enviable position of having some extra doses in this first phase — enough that they recently distributed shots to 75 high-risk teachers. But Elliott says they’re trying not to get too far ahead of surrounding counties or the state of Washington’s phased distribution plan.
“The appearance isn’t good when a health care worker at a busy hospital in Seattle can’t get vaccine and we’re offering it to teachers just so we don’t waste vaccine,” Elliott says.
This speaks to the huge variability in availability from even just one county to the next. And it’s why public health officials are cautioning against reading too much into these apparent, early rural success stories.
Recent Centers for Disease Control and Prevention figures do show that rural states such as Maine, Montana, West Virginia and the Dakotas have led the nation in per capita vaccine distributions. But that may only be because those states are reporting numbers more quickly.
According to the National Rural Health Association, 40% of all rural hospitals in Texas still say they have no access to any of the shots. Morgan, the association’s CEO, says health care providers need the federal government to be more transparent and share data so they can figure out what’s working and isn’t.
ALSO SEE: Coronavirus News, Updates, Resources From NWPB
The outgoing Trump administration has largely left the pandemic management up to states.
“What I’m really concerned about is, going forward into April and May when the general populations can obtain this, where will rural be at that point,” Morgan says.
He worries rural America may continue to be hit harder than its urban counterparts when it comes to hospitalizations and deaths from COVID-19.















