Crisis Clinicians Ride Along With Washington Deputies In Latest Example Of Policing Reimagined
READ ON
In a newly launched pilot project, civilian mental health crisis responders are riding alongside Skagit County, Washington, sheriff’s deputies on 911 calls. It’s the latest example of reimagining policing in the Pacific Northwest.
Skagit County Sheriff’s Office Detective Anne Weed broached the idea for a partnership months before the killing of George Floyd by Minneapolis police ignited the national debate about reform. Weed said two existing mental health clinicians from Compass Health are now being “embedded” with regular patrol deputies. They get assigned the 911 calls involving people acting out who may have mental health problems or addiction issues.

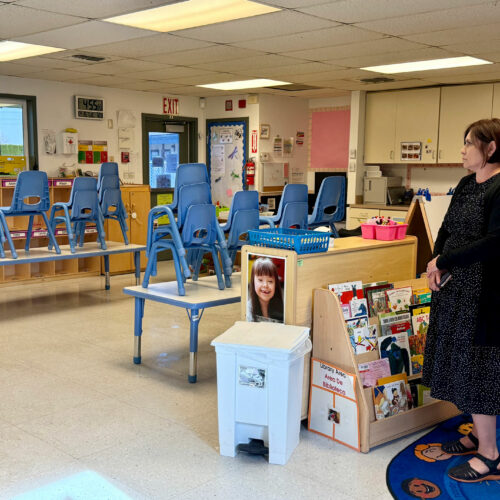
Compass Health program manager Marla Johns, center, and Skagit County Detective Anne Weed, right, collaborated to embed mental health clinicians with deputies responding to relevant 911 calls.
“911 is the number that people call when they need help because that’s the only number that people know when they need help,” Weed said in an interview from the sheriff’s office in Mount Vernon. “In law enforcement, we do have mental health training and de-escalation training, but we’re not clinicians.”
Among the goals of the partnership with Compass Health, a major provider of psychiatric and substance abuse treatment services in Northwest Washington, is to reduce arrests of people caught in a cycle of homelessness, hospitalization and jail. As elsewhere, a small cohort of chronically and pervasively mentally ill people account for a disproportionately high number of police contacts.
“Without a clinician on scene, we would give them a card and say, ‘You can call this number or you can call this person and they’ll offer services for you,'” Weed said. “But when you just hand somebody a card, the likelihood of that person calling is very slim.”
The Skagit County model is a little different than others in this vein regionally — in Eugene-Springfield, Seattle and Olympia, for example — in that the clinician and sheriff’s deputy respond to calls together in the same patrol car. Alternative models have dispatchers deploy an unarmed case worker instead of an officer to certain calls.
Embedding with the deputies enables responses to a wider range of clientele and provides safety to the mental health clinicians in sketchy situations involving suicidal subjects, paranoia or people threatening domestic violence, according to Marla Johns, who manages Compass Health’s mental health crisis response team in Skagit County.
“I don’t want to be the police. That’s not what my area of expertise is,” said Johns. “I want somebody however with me whose experience and expertise is in scene safety, assessment of the environment and making sure things in that way are stable so I can do my job.”
Weed and Johns received funding for two mental clinicians to start off with on the sheriff’s office embed project. Those two positions provide coverage ten hours per day, seven day a week for mental health-related 911 calls in the unincorporated parts of Skagit County. The mental health responders wear civilian clothes to distinguish themselves from law enforcement and lessen the anxiety of the person drawing their attention.
Other models look like this:
CAHOOTS in Eugene-Springfield, Oregon, may be the granddaddy of projects to divert some 911 calls to a more suitable social service response. Run by the nonprofit White Bird Clinic, the 30-year-old program deploys a civilian medic and a trained crisis worker to patrol the mid-sized cities for people in obvious behavioral distress as well as to respond to 911 dispatch referrals of non-criminal crises. Oregon U.S. Senator Ron Wyden recently introduced the CAHOOTS Act to replicate the model nationwide.
In Seattle, Mayor Jenny Durkan on Monday proposed expanding Health One, a program launched in 2019 that’s attached to the fire department instead of the police department. Health One pairs two firefighter EMTs with a social worker who respond together in one rig to non-emergency calls. Their objective is to address the root causes of distress for frequent callers to 911 and other people reported as being in a non-life threatening crisis.
In Olympia, Washington, the two-year-old Crisis Response Unit deploys unarmed mental health specialists to patrol the city’s downtown area. The social workers primarily focus on helping people on the streets with chronic mental health disorders or drug addictions. CRU team members are sometimes dispatched to 911 calls instead of a police officer, especially in situations where a softer approach may result in more cooperation from the subject of the call. If the assistance of a uniformed officer is needed, it’s only a radio call away. The project is a partnership between the Olympia Police Department and Recovery Innovations International.
Compass Health has also worked with the Whatcom County Sheriff’s Office to refine the response to certain categories of 911 calls. In the case of that department, the sheriff chose yet another approach, which was to hire specially-trained “mental health deputies.” Compass Health’s own mobile mental health crisis responders are tied in with the county’s 911 center in Bellingham, but drive around separately and are less tightly integrated than now in neighboring Skagit County.
In the Skagit Valley, Compass Health managers said they have already heard interest from city police departments about joining the mental health embed project just started by their county sheriff’s office.
“In a roundabout way, we are in tune with the moment,” said Brandon Foister, clinical director for crisis response and stabilization for Everett-based Compass Health.
The pilot project in Skagit County is authorized through the middle of next year, but Weed and Marla are already so pleased with how it is going, they anticipate it will be extended. The embedding of mental health clinicians with sheriff’s patrol deputies is funded with a combination of state and county health care dollars and general tax revenues.
Related Stories:

Voucher program provides free counseling for farmers
Washington State University offers a Farm Stress Counseling Voucher program for farmers. Roni Ryan, pictured, is one of the farmers who has received counseling from the program. (Courtesy: Roni Ryan)

Bills to allow some, regulated access to psilocybin unlikely to move forward
Washington state lawmakers still can’t pass bills to allow for some legal access to psychedelics.
With Feb. 21 as the cutoff for bills to move out of policy committees, two pieces of legislation that would have allowed regulated and supervised access to psilocybin for adults won’t be moving forward — Senate Bill 5201 and House Bill 1433. The bills faced opposition from state psychiatric and medical groups, as well as advocates for psychedelics.

‘It’s a crisis’: How the shortage of counselors is affecting the rural Northwest
In small towns, such as Walla Walla, Washington, behavioral health care providers can be hard to come by. (Credit: Susan Shain / NWPB) watch Listen (Runtime 3:49) Read By Rachel