Rural Hospitals Brace For Coronavirus Impacts. Here’s How Grangeville, Idaho Is Preparing
Listen
BY KIRK SIEGLER
In Grangeville, Idaho, population 3,000, Syringa Hospital has just 15 beds, an emergency room and a clinic. As is common in rural medicine, the chief medical officer, Dr. Matthew Told, is also a family practice OB and, on a recent evening, the on-call ER doc.
“We don’t have ventilator services, we don’t have respiratory therapy,” Told says during a break between seeing patients.
WATCH: Getting 2-Weeks Ready Applies To COVID-19 As Well As Earthquakes – Uniquely NW News
There is no intensive care unit. So when they do get a critically ill patient or trauma victims, it’s standard protocol to stabilize and transfer them to a large regional hospital in western Montana or Spokane, Wash. But what if ICUs in those places become overwhelmed with coronavirus patients?
“The biggest challenge is living so close to a state where there are so many cases, such as Washington, and having that really just across the border,” Told says.
Told knows that his hospital could soon be completely overwhelmed and unable to effectively treat anyone, coronavirus patient or not. This is the story in many communities right now. But it could have an even more dire effect in isolated rural towns like this that lack the infrastructure or trained staff, especially if they were to get sick and couldn’t come to work.
Syringa is one of Grangeville’s largest employers.
“If the places that you rely on to send your critically ill patients are full, then you’re stuck,” says Dr. Mark Deutchman, associate dean for rural health at the University of Colorado’s medical school.
Deutchman says people living in more isolated rural areas may be less at risk for contracting the virus because of the sheer lack of people or large gatherings, yet the lack of resources is a perennial challenge during any public health crisis.
Hospital officials in Grangeville say dealing with obstacles and getting creative is a fact of life in rural medicine. For now, their triage plan is to likely block off the ER from the rest of the hospital via a plastic wall. That would at least give them two more isolation beds. They’re also asking patients who may show symptoms of COVID-19 to stay in their cars outside the ER initially, where they can be evaluated and masked.
Michelle Schaeffer, the director at the Syringa clinic, says the single biggest concern right now is they only have about a month’s supply left of masks.

Michelle Schaeffer, director of Syringa Clinics in Idaho, says her facility and an adjoining hospital have about a month’s supply of masks left. CREDIT: Kirk Siegler/NPR
“It doesn’t help that we go to — what is it, an hour and a half to Lewiston? — to our nearest Walmart and there’s not even toilet paper on the shelves because people are panicking,” she says.
So they’re pushing what they see as their most effective tool still at their disposal to fight the spread of the virus in their community: prevention. “So that it never actually gets into the walls of this hospital,” Schaeffer says.
Hospital staff armed with pamphlets and prevention talking points are visiting local businesses, nursing homes and schools. Schools are often the center of small-town life, but they’re also a petri dish for spreading viruses, says Nathan Winder, a physician assistant who sits on Syringa’s infection prevention committee.
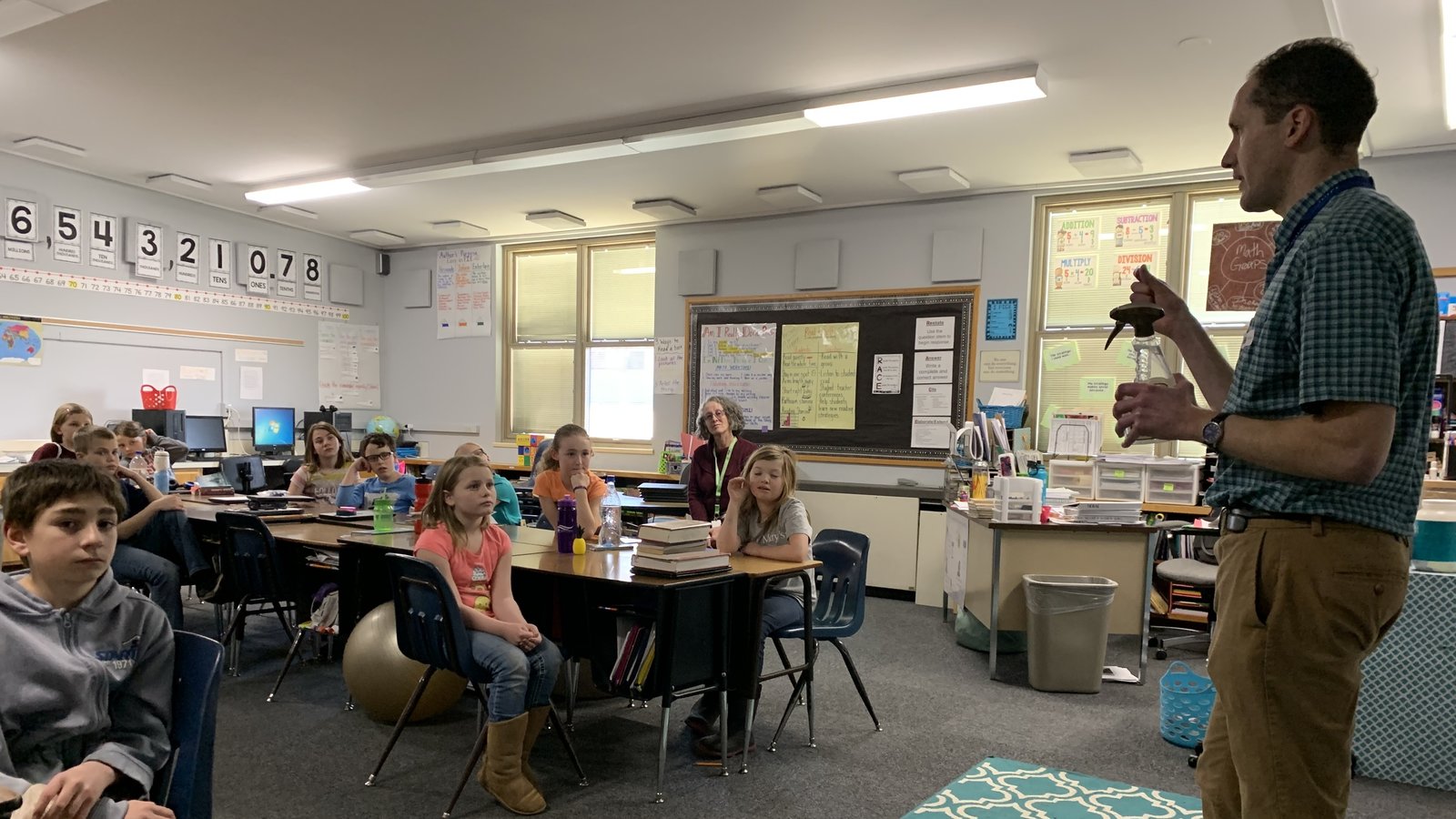
One recent afternoon, clutching a spray bottle as a prop, Winder demonstrated hygiene to an attentive class of fourth-graders at Grangeville Elementary. Most of the kids were aware of the coronavirus, and several said they were already touching elbows instead of doing hand shakes or high fives. Some also boasted they knew to sing most of the popular Baby Shark song while washing their hands.
“And when you cough, cover it with your elbow,” Winder reminded them.
Many of the prevention protocols are similar to what health experts already push during bad influenza outbreaks. Winder left the class feeling encouraged.
WATCH: Getting 2-Weeks Ready Applies To COVID-19 As Well As Earthquakes – Uniquely NW News
“The kids already know a lot,” he said. “You can tell they want to do the right thing, they want to not spread the germs, they don’t want to get sick, they’ve all been sick.”
But hospital officials say this may be the easiest demographic to convince that there is a serious health crisis looming. Like in a lot of rural America, Grangeville’s population skews older. You’ll also tend to find an inherent mistrust toward institutions and the government in rural Idaho, where there are already lower than average vaccination rates.
Conspiracy theories and misinformation are said to be spreading like wildfire on social media. And it’s clear some people just aren’t that worried.
Outside Cloninger’s Supermarket, Jennifer Rogers said she sees the coronavirus as just another bad flu with inconvenient symptoms.
“To me, it feels political,” Rogers says. “It’s an election year and there’s always something big that happens during an election year.”
For now, Rogers said she isn’t doing anything out of the ordinary to prepare.
“I mean, if it were close to home and I knew somebody and I could see their reactions and it was super bad, then it would obviously heighten my awareness,” she said.
But nearby, Gail Solveria traded a handshake for an elbow bump and said she was stocking up with a two-week supply of groceries and medicine should there be a need to isolate. People around here are used to having to be prepared for things like bad weather, she said. And Solveria works as a caregiver for a 93-year-old man.
“We’re trying not to fear, you know, and stay level-headed and trust in God,” she said.
Copyright 2020 NPR. To see more, visit npr.org
Related Stories:

COVID-19, 5 years later: Reflections on the scars we carry, and resilience in unprecedented times
NWPB caught up with local residents and doctors to talk about how they’ve moved forward following the COVID-19 pandemic. They spoke about how the experience changed them and wisdom they’ve gleaned along the way. These are their reflections.
US Supreme Court will consider petition for stay in COVID-19 free speech case
The U.S. Supreme Court will review an application for a stay in a federal lawsuit involving local retired eye doctor Richard Eggleston.
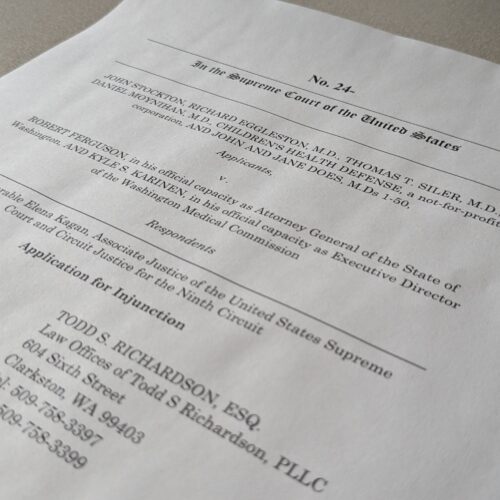
Group representing retired Clarkston ophthalmologist asks US Supreme Court for injunctive relief
A retired Clarkston eye doctor is part of a group asking the U-S Supreme Court to grant an injunction in a lawsuit against Washington state officials.