Lobbying Pays Off: Washington Health Insurers Benefit From Change To Consumer-Focused Bill
READ ON
Strong opposition and intense lobbying by Washington’s health insurance industry has resulted in a key change to a consumer-oriented measure designed to address rising premium costs.
The proposal from Democratic state Sen. Christine Rolfes originally aimed to require the state’s Office of Insurance Commissioner (OIC) to factor in a company’s surplus funds when deciding if a proposed rate increase was reasonable.
In recent years, the state’s three largest nonprofit health insurers – Regence BlueShield, Premera Blue Cross and Kaiser Foundation Health Plan of Washington – have amassed nearly $4.5 billion in surpluses. At the same time, consumers have faced double-digit premium increases.
But on Monday evening, Rolfes’ bill was amended on the floor of the state Senate to change the surplus review requirement to make it optional — not mandatory.
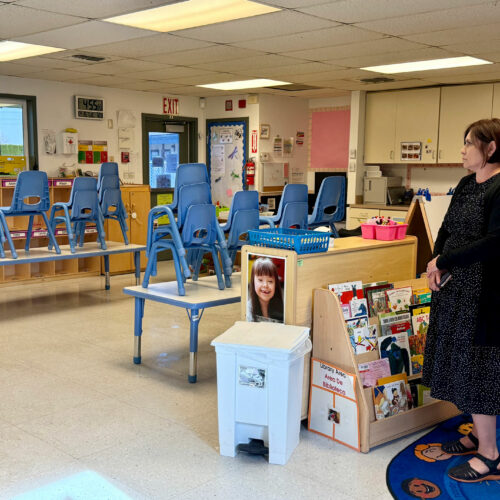
Kaiser Permanente’s Kaiser Foundation Health Plan of Washington is among the largest insurance plans in the state, along with Regence BlueShield and Premera Blue Cross. Together they’ve amassed nearly $4.5 billion in surpluses. At the same time, consumers have faced double-digit premium increases. Courtesy of Kaiser Permanente
“If it sounds like the insurance commissioner’s office and the carriers worked on this amendment together, that’s because they did,” Rolfes acknowledged as she formally introduced the amendment.
It’s not unusual for industry groups to work with regulators and lawmakers on bill language. However, it is rare to hear a state lawmaker speak so candidly about the behind-the-scenes role lobbyists play in Olympia.
In an interview Tuesday, Rolfes defended the new language which she said had been agreed upon just hours before the vote.
“I don’t think [the bill] got gutted at all,” Rolfes said in response to a question about the effects of the amendment.
In fact, Rolfes argued her bill got stronger, not weaker, because the amendment also expanded the scope of the legislation to capture for-profit insurers, which were previously not included.
“The bill as it passed of the Senate floor unanimously encompasses all of the insurance carriers in the state as opposed to just the not-for-profit carriers and so therefore we gave the OIC greater authority to regulate and protect us from unwarranted premium increases,” said Rolfes who serves as chair of the Senate Ways and Means Committee.
In addition to pleasing health insurers, the changes to the bill on the floor of the Senate also won the support of minority Republicans.
“I think there’s been significant material improvements on this bill,” said Republican state Sen. Steve O’Ban in brief comments on the floor before the vote.
Christopher Bandoli is the executive director of the Association of Washington Healthcare Plans. He said after Rolfes’ bill passed out of committee earlier this month, his members discussed what changes could be made to the language to “make it something we can live with.”
Out of those conversations, he said, came an agreement that all health insurers — not just the nonprofits — should be included “for a level playing field.”
“We think that the bill was changed in ways that make it fairer,” Bandoli said.
But that doesn’t mean the health insurance industry will now throw its support behind the bill as it moves to the Washington House. Instead, Bandoli said, his members will now sign-in as “neutral” instead of “opposed.”
Related Stories:

Regence patients could lose coverage at local hospitals, cancer clinic
Two hospitals serving mostly rural areas in Idaho could become more expensive for patients with a major health insurance provider.
Kaiser: Some small group plans will still have First Fill requirement
Kaiser Permanente is set to remove its First Fill requirement for large group plans in Washington next year. However, the program will remain in place for some small group plans. Rachel Sun reports.

Local pharmacists worry for future as more patients switch to mail order
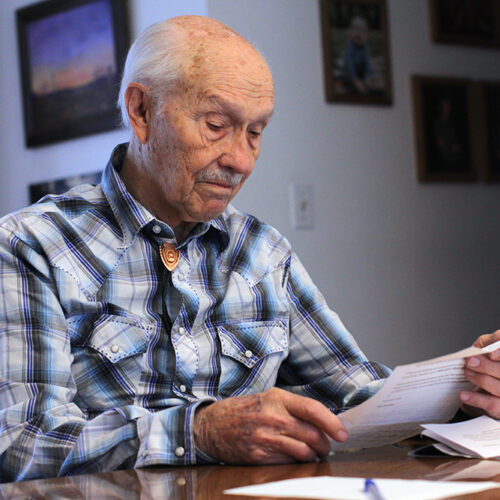
Deborah Beckett sits at a table with her husband Geoff’s prescriptions. Geoff, who is unable to walk due to his Parkinson’s, rests in a bed behind her. Photo by Rachel