
Amid Opioid Crisis, Washington State Looks To Treatment Alternatives
Listen
At a medical clinic in Seattle, Dr. Heather Tick takes a thin acupuncture needle and inserts it into Hannah Lilly’s neck.
“How are you through there?” Dr Tick asks Lilly.
“Not great,” Lilly replies.
She manipulates the needle into the underlying muscle. Then, she turns to Lilly’s back. A class of medical students watches and learns.
“You have to know some anatomy to do any kind of acupuncture needling,” Dr. Tick tells them, “but especially for this one.”
She prods the needle deep into Lilly’s muscles in a procedure called ‘intramuscular stimulation therapy’ or ‘dry needling.’ The work uses the needles to release muscle tension and alleviate chronic pain. It looks uncomfortable.
But afterward, Lilly feels a lot better.
“I can move my head,” she said. “And I feel that there’s a tremendous amount of relief.”
For Lilly, it’s a better alternative than opioids. The drugs had unexpected side effects and only numbed her pain without eliminating it.
“When it comes back after the pain medication wears off, it’s actually worse than it was in the first place,” Lilly said. “So you end up taking more pain medication and being less functional and it’s just a vicious cycle that goes downhill fast.”
“I’ve had several family members and friends that have gone through chronic pain for various reasons and several of them end up addicted to opioids and because they’re still in pain they’re still given drugs that are killing them.”
The opioid epidemic has torn through the United States in recent years. Washington state has not been spared. In 2016, more than 42,000 people died from opioid overdoses, according to the Centers for Disease Control and Prevention. Almost 700 of those deaths were in Washington, according to the state Department of Health.
This has spurred a movement in medicine to find alternatives. Many in the medical profession are more open to using non-opioid drugs that are safer.
“Now we’re starting to recognize that there is a role for the non-pharmacologic as well,” Dr. Tick said. “We don’t just need to substitute one drug for another, necessarily.”
Dr. Tick, a professor of anesthesiology and pain medicine at the University of Washington School of Medicine, was the lead writer of a report released last month by The Academic Consortium for Integrative Medicine and Health that offers evidence for alternative pain management treatments.
She says treatments like conventional acupuncture, massage, tai chi and yoga can treat various types of post-surgical, acute, chronic and cancer pain.
Members of The Academic Consortium for Integrative Medicine and Health include the University of Washington School of Medicine and the Oregon Health and Science University.
There’s evidence that non-pharmacologic treatments can stand alone or work in combination with medicine, surgery or other evidence-based treatments, Dr. Tick said.
“It’s physiology,” she said. “It’s not people imagining or making it go away in a magical way. It is physiology that works that way.”
But it’s not just the medical community that opened up to these alternative treatments. States across the country have expanded Medicaid programs to cover treatments like acupuncture, massage and yoga.
In January, Ohio expanded Medicaid coverage of acupuncture treatments delivered by non- medical providers for lower back pain and migraines. Medicaid agencies in 11 other states, including Washington and Oregon, have implemented policies to encourage the use of alternative pain management strategies instead of opioids, according to a 2016 survey by the National Academy for State Health Policy.
“We have gone so far as a society towards the convenience of popping a pill, where we think that we can do that with impunity, that there are no consequences,” Dr. Tick said. “We don’t talk about what the alternatives could be.”
At first, Hannah Lilly wasn’t looking for alternatives.
Most of her pain is concentrated in her upper body. She had surgery to treat a hernia, and her vagus nerve was damaged. That’s the longest nerve in the human body, passing through the neck to the abdomen. It regulates internal organs like the heart, lungs and the digestive tract.
“It causes severe pain, raises my blood pressure and can make me pass out,” Lilly said. “It made it so that for the first couple years after my surgery I couldn’t hold my kids on my lap because I couldn’t stand anything touching the front of me.”
Her doctor at the time prescribed opioids — high doses of morphine and tramadol that she says made it impossible to concentrate. She couldn’t work as an airplane mechanic anymore and she couldn’t drive.
She also found it hard to take care of her two toddlers.
“They could sit there and talk to me and I could hardly understand what they were saying.” Lilly said. “Or I’d just not be home mentally. I’d just be sitting there on the couch like ‘okay, wow, four hours has gone by and I haven’t done anything.’”
The drugs also had adverse effects on her health. Lilly said they gave her constant nausea and she developed kidney and liver problems. And the physical stress took a toll on her mental health, she said.
Her search for other options eventually led to Dr. Tick and those long, thin needles. Lilly says they help her pain, enough that she comes to downtown Seattle every two weeks.
The only problem is payment. Health insurance companies may not cover those alternatives any time soon. Lilly’s insurance covers the office visit to Dr. Tick, but not the treatment itself. She pays $80 plus a $25 co-pay and parking costs on every visit.
“They consider it ‘experimental,’” Lilly said. “That was the insurance company’s verbiage, not mine.”
Copyright 2018 Northwest News Network
Related Stories:

State considers closure of residential facilities for people with disabilities
Ever since he started working at Rainier School in Buckley, Washington, Willis McNabb has been hearing that the state was going to close it. This time, he said it feels more real.
“I’ve never been so worried as I am today,” McNabb said.
Since 1991, McNabb has worked at Rainier, which gives people with intellectual and developmental disabilities a place to find community, learn, work and receive comprehensive health treatment.
Federal funds to battle opioid addiction coming to rural western Washington hospitals
For people seeking medication-assisted treatment for substance use disorder in some rural Washington communities, there could soon be more options. Recent grant funding from the U.S. Department of Health and Human Services has been allocated to develop medication-assisted treatment (MAT) at rural clinics.

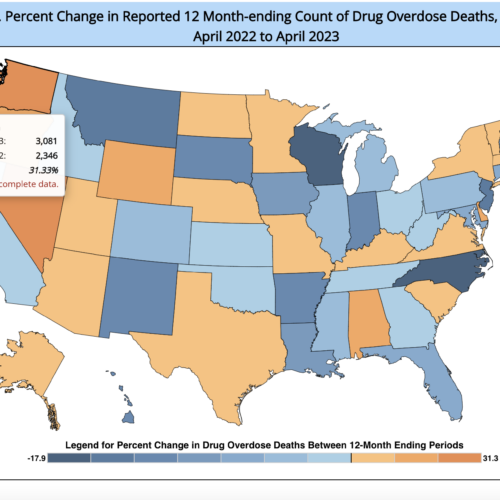
How Washington, Idaho are attempting to reduce increased opioid overdose deaths
In downtown Tacoma, Rachel Ahrens said she sees drug use and abuse frequently.
“I’ve personally seen somebody that was just slumped up against the door and looked to be like an overdose,” said Ahrens, who is the building administrator for First United Methodist Church. “I didn’t have Narcan at that time, so I wasn’t able to administer that. So I had to call 911, for them to help the individual.”

















